Diabetic Retinopathy
Diabetic retinopathy occurs in patients with diabetes mellitus types 1 and 2. Chronically high levels of blood glucose in diabetes can lead to detrimental changes to the blood vessels within the retina. The blood vessels may become leaky and cause swelling in the central retina called diabetic macular edema (DME). With DME, the central vision often becomes blurry. In addition, growth of abnormal blood vessels, a process called neovascularization, may occur. These blood vessels can cause bleeding and scar tissue formation with severe vision loss.
Diabetic macular edema (DME) and neovascularization of the retina may be treated with laser treatment or injections of medications (anti-VEGF) into the eye. Injections of steroids into the eye may also be used to treat DME.
The risk of diabetic retinopathy increases as a diabetic patient ages. After having diabetes for 10 years, approximately 90% of patients will have some evidence of diabetic retinopathy. Therefore, regular dilated eye examinations for all diabetic patients are critical to the early detection of diabetic retinopathy.
There are two types of diabetic retinopathy: non-proliferative retinopathy and proliferative retinopathy. Non-proliferative diabetic retinopathy is the earlier stage and is characterized by visible changes to small retinal blood vessels. If macular edema is not present, then the physician may recommend tight control of the blood sugar and close monitoring of the retina.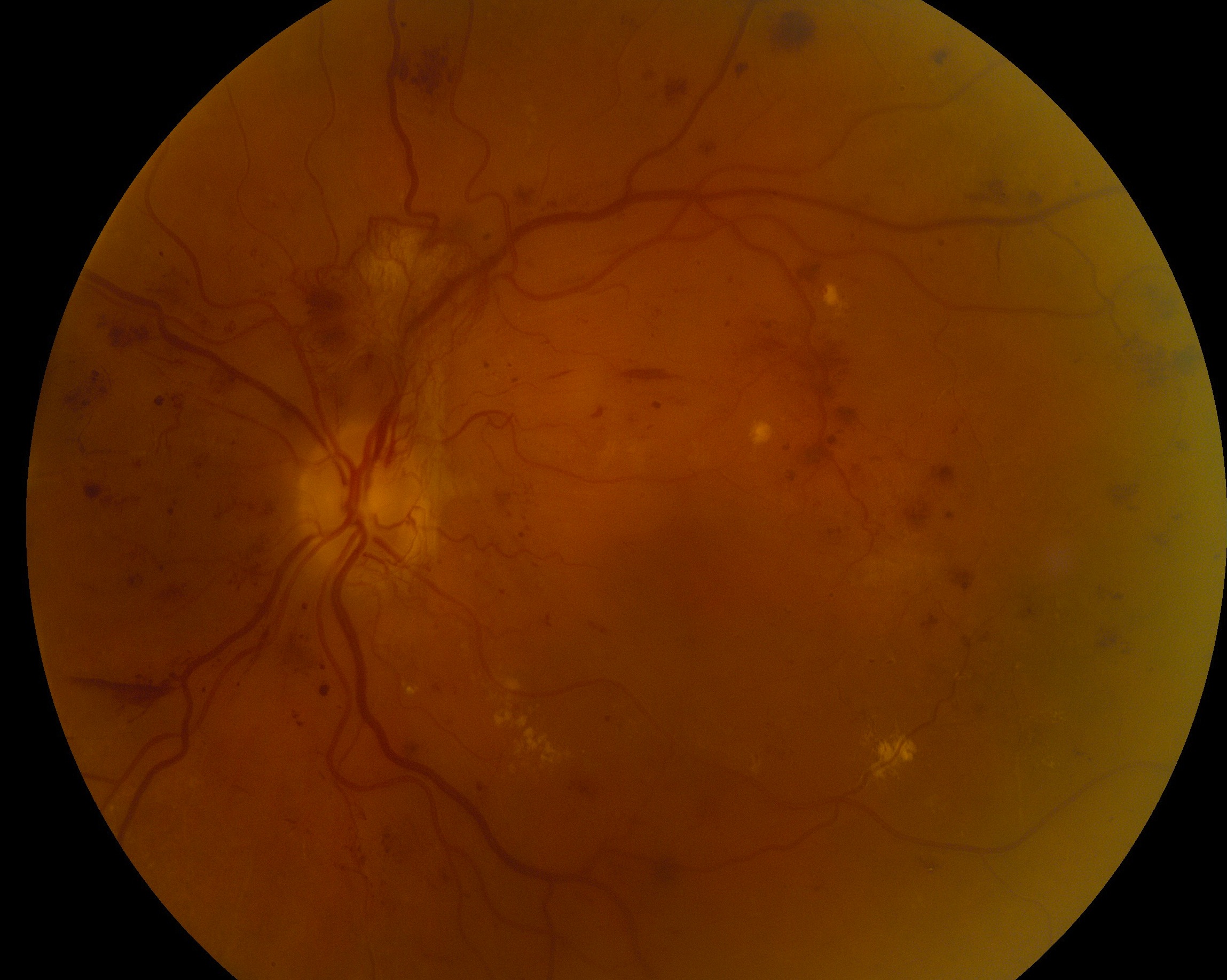
When the retina shows evidence of neovascularization (new blood vessel growth), the patient has developed proliferative diabetic retinopathy, which is a more advanced stage of disease. These abnormal new blood vessels can bleed and cause scar tissue formation. In these cases, treatment may require injection of anti-VEGF medication into the eye, laser treatment, or vitrectomy surgery.